By Maggie Bergeron | Health Swapp
One of the biggest and most significant changes that physiotherapists are currently making is the transition to Electronic Medical Records (EMRs) – “computerized medical information systems that collect, store and display healthcare data about a patient. They allow healthcare professionals to record information about their patients in a legible and organized fashion, as well as creating an efficient method to access the records” (McAllister J. (2014) The financial viability of electronic medical records for private practice physiotherapy in British Columbia (Master’s Thesis).).
EMR and Electronic Health Records (EHR) are often used interchangeably; however, Canada Health Infoway set out a standard definition for each:
- EMR: “a computer-based patient record used in the ambulatory or community setting” (such as a doctor’s or physiotherapist’s clinic).
- EHR: “a lifetime, longitudinal, electronic record of every citizen’s health and their encounters and services received from the healthcare system.”
As you consider making the transition to an EMR system, there are important considerations for your practice and questions you should ask your team and potential vendors.
- Is the EMR PIPEDA compliant (or compliant with the privacy policy for your province)? See my previous blog post about privacy policies.
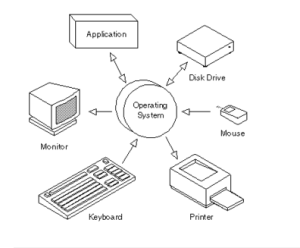
- Is it compatible with the hardware and software in clinic? Consider the following:
- Is there a sufficient number of computers available to support the size of your staff?
- Consider your computer positioning – it’s important to prevent unauthorized viewing.
- Is the operating system that your computer runs on up to date? While most EMR systems will be compatible with the most recent operating systems, they may not support a system that is too old.
o All computers have an operating system (OS) that perform all of the basic computing tasks. It is also responsible for security – making sure unauthorized users don’t access (or hack) your system.
o Some examples of OS are: Microsoft Windows XP, Chrome, Mac OS X Leopard.
o Integrating an EMR in clinic may require additional software components to be installed in order to provide optimization of the system, security and scanning.
- Is your internet connection secure? Also, is the internet available in every area of the clinic where your staff would need to access the EMR system?
- What’s the onboarding process? Learning how to use any new system, whether it’s a new program, new computer or EMR system, takes time but the vendor that you choose should make the process as seamless as possible by working with you. Some questions to consider:
- How long will it take to get started?
- Is training provided?
- What’s the typical length of time for practices to get up and running with the EMR?
- What kind of customer service is provided?
- What support is available during and after implementation?
- Is the support unlimited? Is it free?
- Is there support from live people (ie: over the phone, GoToMeeting or Skype)?
- If I have an issue, how will you help me resolve it?
- It is important that you ask potential EMR vendors what kind of customer support is available, but also consider ahead of time if you will have access to independent tech support. It may be necessary to have additional IT support to help properly install, connect and secure any new hardware or software required for the transition (ie: purchasing new computers, setting up secure internet throughout the clinic, etc).
- What process will you follow to scan current paper charts into the EMR? Or, if you’re switching systems, what’s the process to take electronic files from one system to the other?
- What functions and features are available through the EMR? Here are a few examples of what EMR systems may have to offer:
- Billing
- Scheduling
- Charting
- Manage consents and authorizations
- Capture external clinical documents
- Home exercise software
- Multi-language capabilities
- Statistics and analysis
- Financials
- Reporting
- Marketing and client relationship management
- Staff compensation/salary calculator
- Client web portal
- What is the cost associated with the transition? This includes buying new computers, updating software, additional software required for the EMR system, training staff, the cost of the EMR system, etc.
- Functionality and design matter – this has an effect on the workflow of every staff involved at the clinic from physiotherapists to physiotherapy assistants to administrators. Everyone who is going to use the system should have the opportunity to try the system and voice his or her opinion before fully committing.
The adoption of EMR systems in practice will create efficiencies, provide faster access for providers and better access for patients, ensure professional relevancy, potentially integrate information between care settings and improve research opportunities. However, there are also barriers to the adoption of EMRs including the process of each clinic owner and subsequently their staff learning how to manage the process administratively, technologically, culturally, legislatively, logistically and financially.
The United States and Canada have lagged behind in the adoption of EMR, EHR and health information technology. Many other countries have fully adopted the use of these technologies including the Netherlands, New Zealand and Estonia (who have implemented a nation-wide EHR system). We do not need to re-invent the wheel – we can look to and learn from those who have tested and created systems that are working within their countries.
Evidence informs us that patients and healthcare practitioners value the efficiencies and benefits of EMRs. However, the introduction of technology in practice must be done conscientiously to compliment, not replace the invaluable interpersonal and interprofessional interactions.